From the beginning of recorded history, people have practiced disinfection and sterilization, even though the existence of microorganisms was long unsuspected. The Egyptians used fire to sterilize infectious material and disinfectants to embalm bodies, and the Greeks burned sulfur to fumigate buildings. Mosaic law commanded the Hebrews to burn any clothing suspected of being contaminated with the leprosy bacterium.
Today the ability to destroy microorganisms is no less important: it makes possible the aseptic techniques used in microbiological research, the preservation of food, and the prevention of disease. The techniques described in this chapter are also essential to personal safety in both the laboratory and hospital (Box 7.1).
Definition of Frequently Used Terms
Terminology
is especially important when the control of microorganisms is discussed because
words like disinfectant and antiseptic often are used loosely. The situation is
even more confusing because a particular treatment can either inhibit growth or
kill depending on the conditions.
The
ability to control microbial populations on inanimate objects, like eating
utensils and surgical instruments, is of considerable practical importance.
Sometimes it is necessary to eliminate all microorganisms from an object,
whereas only partial destruction of the microbial population may be required in
other situations.
Sterilization [Latin sterilis, unable to produce offspring or barren] is the process by which all living cells, viable spores, viruses, and viroids are either destroyed or removed from an object or habitat. A sterile object is totally free of viable microorganisms, spores, and other infectious agents. When sterilization is achieved by a chemical agent, the chemical is called a sterilant.
In contrast, disinfection is the killing, inhibition, or removal of microorganisms that may cause disease. The primary goal is to destroy potential pathogens, but disinfection also substantially reduces the total microbial population. Disinfectants are agents, usually chemical, used to carry out disinfection and are normally used only on inanimate objects. A disinfectant does not necessarily sterilize an object because viable spores and a few microorganisms may remain.
Sanitization
is closely related to disinfection. In sanitization, the microbial
population is reduced to levels that are considered safe by public health
standards. The inanimate object is usually cleaned as well as partially
disinfected. For example, sanitizers are used to clean eating utensils in
restaurants.
It is
frequently necessary to control microorganisms on living tissue with chemical
agents. Antisepsis [Greek anti, against, and sepsis, putrefaction]
is the prevention of infection or sepsis and is accomplished with antiseptics.
These are chemical agents applied to tissue to prevent infection by killing
or inhibiting pathogen growth; they also reduce the total microbial population.
Because
they must not destroy too much host tissue, antiseptics are generally not as
toxic as disinfectants.
A
suffix can be employed to denote the type of antimicrobial agent. Substances
that kill organisms often have the suffix –cide [Latin cida, to kill]: a
germicide kills pathogens (and many nonpathogens) but not necessarily
endospores. A disinfectant or antiseptic can be particularly effective against
a specific group, in which case it may be called a bactericide, fungicide,
algicide, or viricide. Other chemicals do not kill, but they do
prevent growth.
If
these agents are removed, growth will resume. Their names end in -static [Greek
statikos, causing to stand or stopping]—for example, bacteriostatic and
fungistatic.
lthough
these agents have been described in terms of their effects on pathogens, it
should be noted that they also kill or inhibit the growth of nonpathogens as
well. Their ability to reduce the total microbial population, not just to
affect pathogen levels, is quite important in many situations.
The Pattern
of Microbial Death
A
microbial population is not killed instantly when exposed to a lethal agent.
Population death, like population growth, is generally exponential or logarithmic—that
is, the population will be reduced by the same fraction at constant intervals (table
7.1).
If
the logarithm of the population number remaining is plotted against the time of
exposure of the microorganism to the agent, a straight line plot will result
(compare figure 7.1 with figure 6.2). When the population has been greatly
reduced, the rate of killing may slow due to the survival of a more resistant strain
of the microorganism.
To
study the effectiveness of a lethal agent, one must be able to decide when
microorganisms are dead, a task by no means as easy as with macro-organisms. It
is hardly possible to take a bacterium’s pulse. A bacterium is defined as dead
if it does not grow and reproduce when inoculated into culture medium that
would normally support its growth. In like manner an inactive virus cannot infect
a suitable host.
Conditions
Influencing the Effectiveness of Antimicrobial Agent Activity
Destruction
of microorganisms and inhibition of microbial growth are not simple matters
because the efficiency of an antimicrobial agent (an agent that kills
microorganisms or inhibits their growth) is affected by at least six factors.
1. Population size. Because an equal fraction of a microbial population is killed during each interval, a larger population requires a longer time to die than a smaller one. This can be seen in the theoretical heat-killing experiment shown in table 7.1 and figure 7.1. The same principle applies to chemical antimicrobial agents.
2. Population composition. The effectiveness of an agent varies greatly with the nature of the organisms being treated because microorganisms differ markedly in susceptibility. Bacterial endospores are much more resistant to most antimicrobial agents than are vegetative forms, and younger cells are usually more readily destroyed than mature organisms. Some species are able to withstand adverse conditions better than others.
Mycobacterium tuberculosis, which causes tuberculosis, is much more resistant to antimicrobial agents than most other bacteria.
3. Concentration or intensity of an antimicrobial agent.
Often, but not always, the more concentrated a chemical agent or intense a physical agent, the more rapidly microorganisms are destroyed. However, agent effectiveness usually is not directly related to concentration or intensity. Over a short range a small increase in concentration leads to an exponential rise in effectiveness; beyond a certain point, increases may not raise the killing rate much at all. Sometimes an agent is more effective at lower concentrations. For example, 70% ethanol is more effective than 95% ethanol because its activity is enhanced by the presence of water.
4. Duration of exposure. The longer a population is exposed to a microbicidal agent, the more organisms are killed (figure 7.1). To achieve sterilization, an exposure duration sufficient to reduce the probability of survival to 10–6 or less should be used.
5. Temperature. An increase in the temperature at which a chemical acts often enhances its activity. Frequently a lower concentration of disinfectant or sterilizing agent can be used at a higher temperature.
6. Local environment. The population to be controlled is not isolated but surrounded by environmental factors that may either offer protection or aid in its destruction.
For example, because heat kills more readily at an acid pH, acid foods and beverages such as fruits and tomatoes are easier to pasteurize than foods with higher pHs like milk. A second important environmental factor is organic matter that can protect microorganisms against heating and chemical disinfectants. Biofilms are a good example.
The organic matter in a surface biofilm will protect the biofilm’s microorganisms; furthermore, the biofilm and its microbes often will be hard to remove. It may be necessary to clean an object before it is disinfected or sterilized. Syringes and medical or dental equipment should be cleaned before sterilization because the presence of too much organic matter could protect pathogens and increase the risk of infection.
The same care must
be taken when pathogens are destroyed during the preparation of drinking water.
When a city’s water supply has a high content of organic material, more
chlorine must be added to disinfect it.
The Use of
Physical Methods in Control
Heat
and other physical agents are normally used to control microbial growth and
sterilize objects, as can be seen from the continual operation of the autoclave
in every microbiology laboratory. The four most frequently employed physical
agents are heat, low temperatures, filtration, and radiation.
Heat
Fire
and boiling water have been used for sterilization and disinfection since the
time of the Greeks, and heating is still one of the most popular ways to
destroy microorganisms. Either moist or dry heat may be applied.
Moist
heat readily kills viruses, bacteria, and fungi (table 7.2). Exposure to
boiling water for 10 minutes is sufficient to destroy vegetative cells and
eucaryotic spores. Unfortunately the temperature of boiling water (100°C or
212°F) is not high enough to destroy bacterial endospores that may survive hours
of boiling.
Therefore
boiling can be used for disinfection of drinking water and objects not harmed
by water, but boiling does not sterilize.
Because
heat is so useful in controlling microorganisms, it is essential to have a
precise measure of the heat-killing efficiency.
Initially
effectiveness was expressed in terms of thermal death point (TDP), the lowest
temperature at which a microbial suspension is killed in 10 minutes. Because
TDP implies that a certain temperature is immediately lethal despite the
conditions, thermal death time (TDT) is now more commonly used. This is the
shortest time needed to kill all organisms in a microbial suspension at a
specific temperature and under defined conditions.
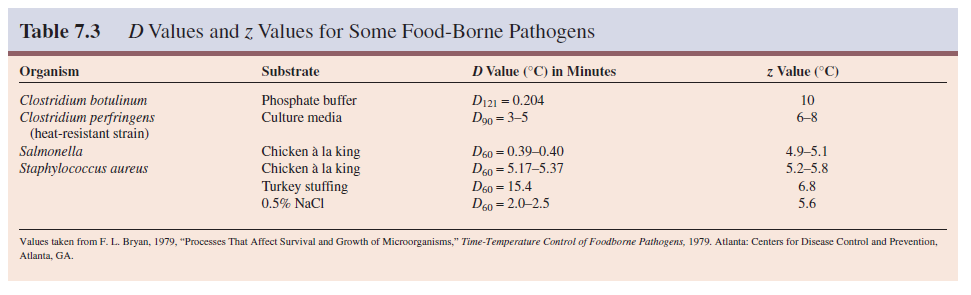
However, such destruction is logarithmic, and it is theoretically not possible to “completely destroy” microorganisms in a sample, even with extended heating. Therefore an even more precise figure, the decimal reduction time (D) or D value has gained wide acceptance. The decimal reduction time is the time required to kill 90% of the microorganisms or spores in a sample at a specified temperature. In a semilogarithmic plot of the population remaining versus the time of heating (figure 7.1), the D value is the time required for the line to drop by one log cycle or tenfold.
The D value is usually
written with a subscript, indicating the temperature for which it applies. D
values are used to estimate the relative resistance of a microorganism to
different temperatures through calculation of the z value. The z value
is the increase in temperature required to reduce D to 1/10 its value or
to reduce it by one log cycle when log D is plotted against temperature
(figure 7.2). Another way to describe heating effectiveness is with the F value.
The F value is the time in minutes at a specific temperature (usually
250°F or 121.1°C) needed to kill a population of cells or spores.
The food processing industry makes extensive use of D and z values. After a food has been canned, it must be heated to eliminate the risk of botulism arising from Clostridium botulinum spores. Heat treatment is carried out long enough to reduce a population of 1012 C. botulinum spores to 100 (one spore); thus there is a very small chance of any can having a viable spore. The D value for these spores at 121°C is 0.204 minutes.
Therefore it would take 12D or 2.5 minutes to reduce 1012 spores to one spore by heating at 121°C. The z value for C. botulinum spores is 10°C—that is, it takes a 10°C change in temperature to alter the D value tenfold. If the cans were to be processed at 111°C rather than at 121°C, the D value would increase by tenfold to 2.04 minutes and the 12D value to 24.5 minutes. D values and z values for some common food-borne pathogens are given in table 7.3. Three D values are included for Staphylococcus aureus to illustrate the variation of killing rate with environment and the protective effect of organic material.
Moist heat sterilization must be carried out at temperatures above 100°C in order to destroy bacterial endospores, and this requires the use of saturated steam under pressure. Steam sterilization is carried out with an autoclave (figure 7.3), a device somewhat like a fancy pressure cooker. The development of the autoclave by Chamberland in 1884 tremendously stimulated the growth of microbiology. Water is boiled to produce steam, which is released through the jacket and into the autoclave’s chamber.
The air initially present in the chamber is forced out until the chamber is
filled with saturated steam and the outlets are closed. Hot, saturated steam
continues to enter until the chamber reaches the desired temperature and
pressure, usually 121°C and 15 pounds of pressure.
At
this temperature saturated steam destroys all vegetative cells and endospores
in a small volume of liquid within 10 to 12 minutes. Treatment is continued for
about 15 minutes to provide a margin of safety. Of course, larger containers of
liquid such as flasks and carboys will require much longer treatment times.
 |
Moist
heat is thought to kill so effectively by degrading nucleic acids and by
denaturing enzymes and other essential proteins.
It also may disrupt cell membranes. Autoclaving must be carried out properly or the processed materials will not be sterile. If all air has not been flushed out of the chamber, it will not reach 121°C even though it may reach a pressure of 15 pounds. The chamber should not be packed too tightly because the steam needs to circulate freely and contact everything in the autoclave.
Bacterial endospores
will be killed only if they are kept at 121°C for 10 to 12 minutes. When a
large volume of liquid must be sterilized, an extended sterilization time will
be needed because it will take longer for the center of the liquid to reach
121°C; 5 liters of liquid may require about 70 minutes.
In view of these potential difficulties, a biological indicator is often autoclaved along with other material. This indicator commonly consists of a culture tube containing a sterile ampule of medium and a paper strip covered with spores of Bacillus stearothermophilus or Clostridium PA3679. After autoclaving, the ampule is aseptically broken and the culture incubated for several days.
If the test bacterium does not grow in the medium, the
sterilization run has been successful. Sometimes either special tape that
spells out the word sterile or a paper indicator strip that changes
color upon sufficient heating is autoclaved with a load of material. If the
word appears on the tape or if the color changes after autoclaving, the
material is supposed to be sterile.
These approaches are convenient and save time but are not as reliable as the use of bacterial endospores. Many substances, such as milk, are treated with controlled heating at temperatures well below boiling, a process known as pasteurization in honor of its developer Louis Pasteur. In the 1860s the French wine industry was plagued by the problem of wine spoilage, which made wine storage and shipping difficult.
Pasteur examined spoiled wine under the microscope and detected microorganisms that looked like the bacteria responsible for lactic acid and acetic acid fermentations. He then discovered that a brief heating at 55 to 60°C would destroy these microorganisms and preserve wine for long periods. In 1886 the German chemists V. H. and F. Soxhlet adapted the technique for preserving milk and reducing milk transmissible diseases.
Milk pasteurization
was introduced into the United States in 1889. Milk, beer, and many other
beverages are now pasteurized. Pasteurization does not sterilize a beverage,
but it does kill any pathogens present and drastically slows spoilage by
reducing the level of nonpathogenic spoilage microorganisms.
Milk
can be pasteurized in two ways. In the older method the milk is held at 63°C
for 30 minutes. Large quantities of milk are now usually subjected to flash
pasteurization or high-temperature short-term (HTST) pasteurization, which
consists of quick heating to about 72°C for 15 seconds, then rapid cooling. The
dairy industry also sometimes uses ultrahigh-temperature (UHT) sterilization. Milk
and milk products are heated at 140 to 150°C for 1 to 3 seconds. UHT-processed
milk does not require refrigeration and can be stored at room temperature for
about 2 months without flavor changes. The small coffee creamer portions provided
by restaurants often are prepared using UHT sterilization.
Many objects are best sterilized in the absence of water by dry heat sterilization. The items to be sterilized are placed in an oven at 160 to 170°C for 2 to 3 hours. Microbial death apparently results from the oxidation of cell constituents and denaturation of proteins. Although dry air heat is less effective than moist heat— Clostridium botulinum spores are killed in 5 minutes at 121°C by moist heat but only after 2 hours at 160°C with dry heat—it has some definite advantages.
Dry heat does not corrode glassware and metal instruments as moist
heat does, and it can be used to sterilize powders, oils, and similar items.
Most laboratories sterilize glass petri dishes and pipettes with dry heat. Despite
these advantages, dry heat sterilization is slow and not suitable for heat sensitive
materials like many plastic and rubber items.
Low
Temperatures
Although
our emphasis is on the destruction of microorganisms, often the most convenient
control technique is to inhibit their growth and reproduction by the use of
either freezing or refrigeration.
This
approach is particularly important in food microbiology. Freezing items at -20°C
or lower stops microbial growth because of the low temperature and the absence
of liquid water. Some microorganisms will be killed by ice crystal disruption
of cell membranes, but freezing does not destroy contaminating microbes. In
fact, freezing is a very good method for long-term storage of microbial samples
when carried out properly, and many laboratories have a low-temperature freezer
for culture storage at -30 or -70°C. Because frozen food can contain many
microorganisms, it should be prepared and consumed promptly after thawing in
order to avoid spoilage and pathogen growth.
Refrigeration
greatly slows microbial growth and reproduction, but does not halt it
completely. Fortunately most pathogens are mesophilic and do not grow well at
temperatures around 4°C.
Refrigerated
items may be ruined by growth of psychrophilic and psychrotrophic
microorganisms, particularly if water is present.
Thus
refrigeration is a good technique only for shorter-term storage of food and
other items.
Filtration
Filtration is an excellent way to reduce the microbial population in solutions of heat-sensitive material, and sometimes it can be used to sterilize solutions. Rather than directly destroying contaminating microorganisms, the filter simply removes them. There are two types of filters. Depth filters consist of fibrous or granular materials that have been bonded into a thick layer filled with twisting channels of small diameter.
The solution containing microorganisms is
sucked through this layer under vacuum, and microbial cells are removed by
physical screening or entrapment and also by adsorption to the surface of the
filter material. Depth filters are made of diatomaceous earth (Berkefield
filters), unglazed porcelain (Chamberlain filters), asbestos, or other similar
materials.
Membrane
filters have replaced depth filters for many purposes. These circular filters
are porous membranes, a little over 0.1 mm thick, made of cellulose acetate,
cellulose nitrate, polycarbonate, polyvinylidene fluoride, or other synthetic
materials.
Although
a wide variety of pore sizes are available, membranes with pores about 0.2 µm
in diameter are used to remove most vegetative cells, but not viruses, from
solutions ranging in volume from 1 ml to many liters. The membranes are held in
special holders (figure 7.4) and often preceded by depth filters made of glass fibers
to remove larger particles that might clog the membrane filter.
The
solution is pulled or forced through the filter with a vacuum or with pressure
from a syringe, peristaltic pump, or nitrogen gas bottle, and collected in
previously sterilized containers. Membrane filters remove microorganisms by
screening them out much as a sieve separates large sand particles from small
ones (figure 7.5).
These
filters are used to sterilize pharmaceuticals, ophthalmic solutions, culture
media, oils, antibiotics, and other heat-sensitive solutions.
Air also can be sterilized by filtration. Two common examples are surgical masks and cotton plugs on culture vessels that let air in but keep microorganisms out. Laminar flow biological safety cabinets employing high-efficiency particulate air (HEPA) filters, which remove 99.97% of 0.3 µm particles, are one of the most important air filtration systems. Laminar flow biological safety cabinets force air through HEPA filters, then project a vertical curtain of sterile air across the cabinet opening.
This protects a worker from microorganisms being handled
within the cabinet and prevents contamination of the room (figure 7.6). A person
uses these cabinets when working with dangerous agents such as Mycobacterium
tuberculosis, tumor viruses, and recombinant DNA. They are also employed in
research labs and industries, such as the pharmaceutical industry, when a
sterile working surface is needed for conducting assays, preparing media,
examining tissue cultures, and the like.
Radiation
The
types of radiation and the ways in which radiation damages or destroys
microorganisms have already been discussed. The practical uses of ultraviolet
and ionizing radiation in sterilizing objects are briefly described next.
Ultraviolet
(UV) radiation around 260 nm (see figure 6.17) is quite lethal but does
not penetrate glass, dirt films, water, and other substances very effectively.
Because of this disadvantage, UV radiation is used as a sterilizing agent only
in a few specific situations.
UV
lamps are sometimes placed on the ceilings of rooms or in biological safety
cabinets to sterilize the air and any exposed surfaces.
Because
UV radiation burns the skin and damages eyes, people working in such areas must
be certain the UV lamps are off when the areas are in use. Commercial UV units
are available for water treatment. Pathogens and other microorganisms are
destroyed when a thin layer of water is passed under the lamps.
Ionizing radiation is an excellent sterilizing agent and penetrates deep into objects. It will destroy bacterial endospores and vegetative cells, both procaryotic and eucaryotic; however, ionizing radiation is not always as effective against viruses. Gamma radiation from a cobalt 60 source is used in the cold sterilization of antibiotics, hormones, sutures, and plastic disposable supplies such as syringes. Gamma radiation has also been used to sterilize and “pasteurize” meat and other food.
Irradiation can eliminate the threat of such pathogens as Escherichia coli O157:H7, Staphylococcus aureus, and Campylobacter jejuni. Both the Food and Drug Administration and the World Health Organization have approved food irradiation and declared it safe. A commercial irradiation plant operates near Tampa, Florida.
However, this process has not yet been widely employed in
the United States because of the cost and concerns about the effects of gamma
radiation on food. The U.S. government currently approves the use of radiation
to treat poultry, beef, pork, veal, lamb, fruits, vegetables, and spices. It
will probably be more extensively employed in the future.
The Use of
Chemical Agents in Control
Although
objects are sometimes disinfected with physical agents, chemicals are more
often employed in disinfection and antisepsis.
Many
factors influence the effectiveness of chemical disinfectants and antiseptics
as previously discussed. Factors such as the kinds of microorganisms
potentially present, the concentration and nature of the disinfectant to be
used, and the length of treatment should be considered. Dirty surfaces must be
cleaned before a disinfectant or antiseptic is applied. The proper use of chemical
agents is essential to laboratory and hospital safety (Box 7.2; see also Box
36.1). It should be noted that chemicals also are employed to prevent
microbial growth in food. This is discussed in the chapter on food microbiology.
Many
different chemicals are available for use as disinfectants, and each has its
own advantages and disadvantages. In selecting an agent, it is important to
keep in mind the characteristics of a desirable disinfectant. Ideally the
disinfectant must be effective against a wide variety of infectious agents
(gram-positive and gram-negative bacteria, acid-fast bacteria, bacterial
endospores, fungi, and viruses) at high dilutions and in the presence of
organic matter.
Although
the chemical must be toxic for infectious agents, it should not be toxic to
people or corrosive for common materials. In practice, this balance between
effectiveness and low toxicity for animals is hard to achieve. Some chemicals are
used despite their low effectiveness because they are relatively nontoxic. The
disinfectant should be stable upon storage, odorless or with a pleasant odor,
soluble in water and lipids
for
penetration into microorganisms, and have a low surface tension so that it can
enter cracks in surfaces. If possible the disinfectant should be relatively
inexpensive.
One
potentially serious problem is the overuse of triclosan and other germicides.
This antibacterial agent is now found in products such as deodorants,
mouthwashes, soaps, cutting boards, and baby toys. Triclosan seems to be
everywhere. Unfortunately we are already seeing the emergence of
triclosan-resistant bacteria.
Pseudomonas aeruginosa actively pumps the antiseptic out the cell. Bacteria
seem to be responding to antiseptic overuse in the same way as they reacted to
antibiotic overuse. There is now some evidence that extensive use of triclosan
also increases the frequency of antibiotic resistance in bacteria. Thus overuse
of antiseptics can have unintended harmful consequences.
The properties and uses of several groups of common disinfectants and antiseptics are surveyed next. Many of their characteristics are summarized in tables 7.4 and 7.5. Structures of some common agents are given in figure 7.7.
Phenolics
Phenol
was the first widely used antiseptic and disinfectant. In 1867 Joseph Lister
employed it to reduce the risk of infection during operations. Today phenol and
phenolics (phenol derivatives) such as cresols, xylenols, and orthophenylphenol
are used as disinfectants in laboratories and hospitals. The commercial
disinfectant Lysol is made of a mixture of phenolics.
Phenolics
act by denaturing proteins and disrupting cell membranes. They have some real
advantages as disinfectants: phenolics are tuberculocidal, effective in the
presence of organic material, and remain active on surfaces long after
application.
However,
they do have a disagreeable odor and can cause skin irritation. Hexachlorophene
(figure 7.7) has been one of the most popular antiseptics because it persists
on the skin once applied and reduces skin bacteria for long periods. However,
it can cause brain damage and is now used in hospital nurseries only in
response to a staphylococcal outbreak.
Alcohols
Alcohols
are among the most widely used disinfectants and antiseptics. They are bactericidal
and fungicidal but not sporicidal; some lipid-containing viruses are also
destroyed. The two most popular alcohol germicides are ethanol and isopropanol,
usually used in about 70 to 80% concentration. They act by denaturing proteins
and possibly by dissolving membrane lipids. A 10 to 15 minute soaking is
sufficient to disinfect thermometers and small instruments.
Halogens
A halogen is any of the five elements (fluorine, chlorine, bromine, iodine, and astatine) in group VIIA of the periodic table. They exist as diatomic molecules in the free state and form salt-like compounds with sodium and most other metals. The halogens iodine and chlorine are important antimicrobial agents. Iodine is used as a skin antiseptic and kills by oxidizing cell constituents and iodinating cell proteins.
At higher concentrations, it may even kill some
spores. Iodine often has been applied as tincture of iodine, 2% or more iodine in
a water-ethanol solution of potassium iodide. Although it is an effective antiseptic,
the skin may be damaged, a stain is left, and iodine allergies can result. More
recently iodine has been complexed with an organic carrier to form an iodophor.
Iodophors are water soluble, stable, and non staining, and release iodine
slowly to minimize skin burns and irritation. They are used in hospitals for
preoperative skin degerming and in hospitals and laboratories for disinfecting.
Some
popular brands are Wescodyne for skin and laboratory disinfection and Betadine
for wounds.
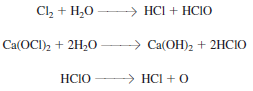
Chlorine
is the usual disinfectant for municipal water supplies and swimming pools and
is also employed in the dairy and food industries. It may be applied as
chlorine gas, sodium hypochlorite, or calcium hypochlorite, all of which yield
hypochlorous acid (HClO) and then atomic oxygen. The result is oxidation of
cellular materials and destruction of vegetative bacteria and fungi, although
not spores.
Death of almost all microorganisms usually occurs within 30 minutes. Since organic material interferes with chlorine action by reacting with chlorine and its products, an excess of chlorine is added to ensure microbial destruction. One potential problem is that chlorine reacts with organic compounds to form carcinogenic trihalomethanes, which must be monitored in drinking water. Ozone sometimes has been used successfully as an alternative to chlorination in Europe and Canada.
Municipal water purification Chlorine is also an excellent disinfectant
for individual use because it is effective, inexpensive, and easy to employ. Small
quantities of drinking water can be disinfected with halazone tablets. Halazone
(parasulfone dichloramidobenzoic acid) slowly releases chloride when added to
water and disinfects it in about a half hour. It is frequently used by campers
lacking access to uncontaminated drinking water.
Chlorine
solutions make very effective laboratory and household disinfectants. An
excellent disinfectant-detergent combination can be prepared if a 1/100
dilution of household bleach (e.g., 1.3 fl oz of Clorox or Purex bleach in 1
gal or 10 ml/liter) is combined with sufficient nonionic detergent (about 1
oz/gal or 7.8 ml/liter) to give a 0.8% detergent concentration. This mixture
will remove both dirt and bacteria.
Heavy Metals
For
many years the ions of heavy metals such as mercury, silver, arsenic, zinc, and
copper were used as germicides. More recently these have been superseded by
other less toxic and more effective germicides
(many heavy metals are more bacteriostatic than bactericidal).
There
are a few exceptions. A 1% solution of silver nitrate is often added to the
eyes of infants to prevent ophthalmic gonorrhea (in many hospitals,
erythromycin is used instead of silver nitrate because it is effective against Chlamydia
as well as Neisseria). Silver sulfadiazine is used on burns. Copper
sulfate is an effective algicide in lakes and swimming pools.
Heavy
metals combine with proteins, often with their sulfhydryl groups, and
inactivate them. They may also precipitate cell proteins.
Quaternary
Ammonium Compounds
Detergents
[Latin detergere, to wipe off or away] are organic molecules that serve
as wetting agents and emulsifiers because they have both polar hydrophilic and
nonpolar hydrophobic ends. Due to their amphipathic nature, detergents
solubilize otherwise insoluble residues and are very effective cleansing agents.
They are different than soaps, which are derived from fats.
Although
anionic detergents have some antimicrobial properties, only cationic detergents
are effective disinfectants.
The
most popular of these disinfectants are quaternary ammonium compounds
characterized by a positively charged quaternary nitrogen and a long
hydrophobic aliphatic chain (figure 7.7). They disrupt microbial membranes and
may also denature proteins.
Cationic
detergents like benzalkonium chloride and cetylpyridinium chloride kill most
bacteria but not M. tuberculosis or endospores.
They
do have the advantages of being stable, nontoxic, and bland but they are
inactivated by hard water and soap. Cationic detergents are often used as
disinfectants for food utensils and small instruments and as skin antiseptics.
Several brands are on the market. Zephiran contains benzalkonium chloride and
Ceepryn, cetylpyridinium chloride.
Aldehydes
Both
of the commonly used aldehydes, formaldehyde and glutaraldehyde, are highly
reactive molecules that combine with nucleic
acids
and proteins and inactivate them, probably by crosslinking and alkylating
molecules (figure 7.7). They are sporicidal and can be used as chemical
sterilants. Formaldehyde is usually dissolved in water or alcohol before use. A
2% buffered solution of glutaraldehyde is an effective disinfectant. It is less
irritating than formaldehyde and is used to disinfect hospital and laboratory
equipment. Glutaraldehyde usually disinfects objects within about 10 minutes
but may require as long as 12 hours to destroy all spores.
Sterilizing Gases
Many
heat-sensitive items such as disposable plastic petri dishes and syringes,
heart-lung machine components, sutures, and catheters are now sterilized with
ethylene oxide gas (figure 7.7). Ethylene oxide (EtO) is both microbicidal and
sporicidal and kills by combining with cell proteins. It is a particularly effective
sterilizing agent because it rapidly penetrates packing materials, even plastic
wraps.
Sterilization
is carried out in a special ethylene oxide sterilizer, very much resembling an
autoclave in appearance, that controls the EtO concentration, temperature, and
humidity. Because pure EtO is explosive, it is usually supplied in a 10 to 20% concentration
mixed with either CO2 or dichlorodifluoromethane.
The
ethylene oxide concentration, humidity, and temperature influence the rate of
sterilization. A clean object can be sterilized if treated for 5 to 8 hours at
38°C or 3 to 4 hours at 54°C when the relative humidity is maintained at 40 to
50% and the EtO concentration at 700 mg/liter. Extensive aeration of the
sterilized materials is necessary to remove residual EtO because it is so
toxic.
Betapropiolactone
(BPL) is occasionally employed as a sterilizing gas. In the liquid form it has
been used to sterilize vaccines and sera. BPL decomposes to an inactive form
after several hours and is therefore not as difficult to eliminate as EtO. It
also destroys microorganisms more readily than ethylene oxide but does not
penetrate materials well and may be carcinogenic. For these reasons, BPL has
not been used as extensively as EtO.
Recently
vapor-phase hydrogen peroxide has been used to decontaminate biological safety
cabinets.
Evaluation of Antimicrobial Agent Effectiveness
Testing of
antimicrobial agents is a complex process regulated by two different federal
agencies. The U.S. Environmental Protection Agency regulates disinfectants,
whereas agents used on humans and animals are under the control of the Food and
Drug Administration.
Testing of
antimicrobial agents often begins with an initial screening test to see if they
are effective and at what concentrations.
This may be
followed by more realistic in-use testing. The best-known disinfectant
screening test is the phenol coefficient test in which the potency of a
disinfectant is compared with that of phenol. A series of dilutions of phenol
and the experimental disinfectant are inoculated with the test bacteria Salmonella
typhi and Staphylococcus aureus, then placed in a 20 or 37°C water
bath.
These
inoculated disinfectant tubes are next subcultured to regular fresh medium at 5
minute intervals, and the subcultures are incubated for two or more days. The
highest dilutions that kill the bacteria after a 10 minute exposure, but not
after 5 minutes, are used to calculate the phenol coefficient. The reciprocal of
the appropriate test disinfectant dilution is divided by that for phenol to
obtain the coefficient. Suppose that the phenol dilution was 1/90 and maximum
effective dilution for disinfectant X was 1/450. The phenol coefficient of X
would be 5.
The higher the
phenol coefficient value, the more effective the disinfectant under these test
conditions. A value greater than 1 means that the disinfectant is more
effective than phenol. A few representative phenol coefficient values are given
in table 7.6.
The phenol
coefficient test is a useful initial screening procedure, but the phenol
coefficient can be misleading if taken as a direct indication of disinfectant
potency during normal use. This is because the phenol coefficient is determined
under carefully controlled conditions with pure bacterial strains, whereas
disinfectants are normally used on complex populations in the presence of
organic matter and with significant variations in environmental factors like
pH, temperature, and presence of salts.
To more
realistically estimate disinfectant effectiveness, other tests are often used.
The rates at which selected bacteria are destroyed with various chemical agents
may be experimentally determined and compared. A use dilution test can also be
carried out.
Stainless
steel cylinders are contaminated with specific bacterial species under
carefully controlled conditions. The cylinders are dried briefly, immersed in
the test disinfectants for 10 minutes, transferred to culture media, and
incubated for two days.
The
disinfectant concentration that kills the organisms in the sample with a 95%
level of confidence under these conditions is determined.
Disinfectants
also can be tested under conditions designed to simulate normal in-use
situations. In-use testing techniques allow a more accurate determination of
the proper disinfectant concentration for a particular situation.













No comments:
Post a Comment